Sitafloxacin demonstrated 100% Chlamydia trachomatis eradication rate among male patients with urethritis in Japan
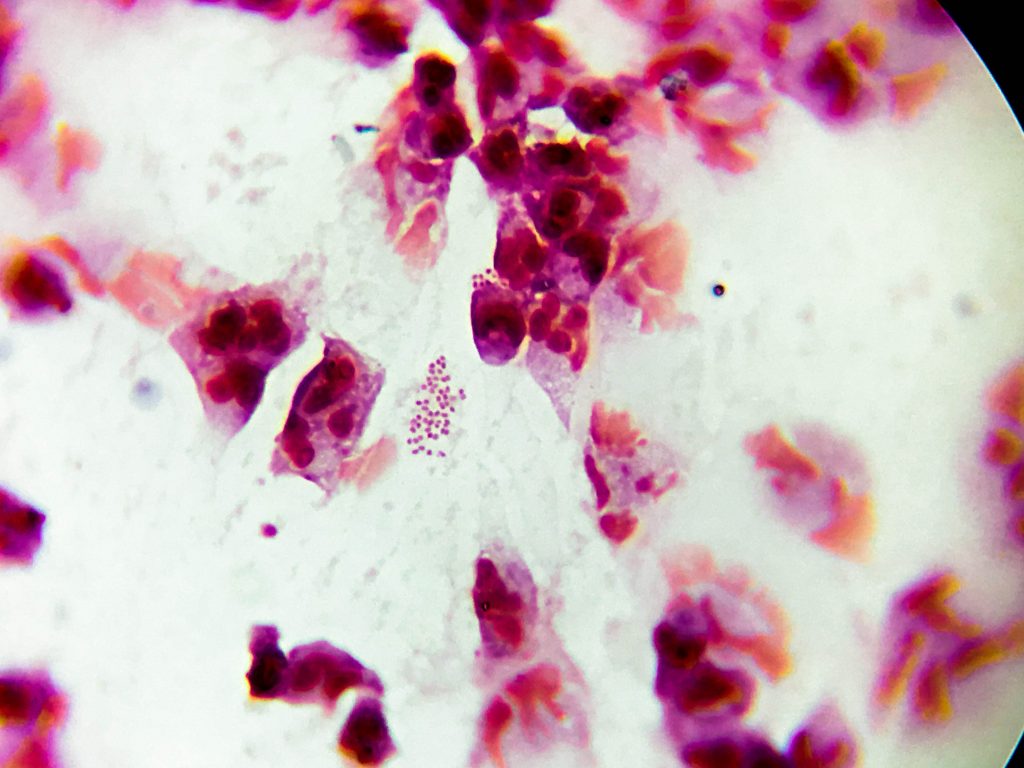
Chlamydia trachomatis is one of the most common causes of non-gonococcal urethritis in men.1 Treatment options for chlamydia urethritis include tetracyclines, macrolides and fluoroquinolones. Drug-resistant C. trachomatis isolates have been reported worldwide but antimicrobial surveillance data remain scarce.2-5 To clarify the status of drug resistance in clinical strains of C. trachomatis, Deguchi and colleagues examined C. trachomatis DNAs from first-void urine specimens from men with acute urethritis. The investigators utilized polymerase chain reaction (PCR) to detect the presence of fluoroquinolone resistance-associated mutations in the gyrA and parC genes and macrolide resistance-associated mutations in the 23S rRNA gene.6
A total of 284 DNA specimens positive for C. trachomatis were obtained from a urologic clinic (iClinic) in Sendai, Japan between April 2013 and December 2016. No mutations were detected in the 23S rRNA gene. Similarly, no mutations were found within the quinolone resistance-determining regions (QRDRs) of the gyrA gene and analogous regions of the parC gene. Amino acid changes of V61A and H129Q were found in the gyrA gene (44 of 118 DNA specimens, 37.3%), but these were not localized in the QRDR. The authors stated that these amino acid changes found outside the QRDR of the gyrA gene do not contribute to the development of fluoroquinolone resistance.
In addition to the PCR analysis of urine samples, a retrospective analysis of clinical data of men complaining of acute urethritis symptoms between January 2013 and June 2017 was also performed. A total of 369 men whose first-void urine specimens were positive for C. trachomatis during their first visits were treated with either azithromycin-SR (2 g once daily for 1 day) or sitafloxacin (100 mg twice daily for 7 days). Outcomes of the antimicrobial therapies were assessed by re-testing the urine samples by APRIMA Combo 2 for C. trachomatis 21 to 60 days after treatment initiation. Of the 314 patients treated with azithromycin-SR, 176 were assessed for microbiological outcomes. Seven patients showed bacterial persistence and were deemed treatment failures. In contrast, of the 55 patients treated with sitafloxacin, 30 patients were assessed for microbiological outcomes. Sitafloxacin conferred 100% eradication rate.
In this study, mutations associated with macrolide or fluoroquinolone resistance were not found in the C. trachomatis DNAs. Given the low treatment failure rate with azithromycin and the 100% eradication rate with sitafloxacin, the authors concluded that both fluoroquinolone and azithromycin regimens can be recommended as treatment of choice for urogenital C. trachomatis infections.
Source:
Macrolide and fluoroquinolone resistance is uncommon in clinical strains of Chlamydia trachomatis.
PMID: 29627327
Link: https://www.ncbi.nlm.nih.gov/pubmed/29627327
References:
- Libois A, Hallin M, Crucitti T, Delforge M, De Wit S. Prevalence of Mycoplasma genitalium in men with urethritis in a large public hospital in Brussels, Belgium: An observational, cross-sectional study. PLoS ONE. 2018;13(4):e0196217.
- Jones RB, Van der Pol B, Martin DH, Shepard MK. Partial characterization of Chlamydia trachomatis isolates resistant to multiple antibiotics. J Infect Dis. Dec 1990;162(6):1309-1315.
- Lefevre JC, Lepargneur JP, Guion D, Bei S. Tetracycline-resistant Chlamydia trachomatis in Toulouse, France. Pathol Biol (Paris). May 1997;45(5):376-378.
- Somani J, Bhullar VB, Workowski KA, Farshy CE, Black CM. Multiple drug-resistant Chlamydia trachomatis associated with clinical treatment failure. J Infect Dis. Apr 2000;181(4):1421-1427.
- Bhengraj AR, Vardhan H, Srivastava P, Salhan S, Mittal A. Decreased susceptibility to azithromycin and doxycycline in clinical isolates of Chlamydia trachomatis obtained from recurrently infected female patients in India. Chemotherapy. 2010;56(5):371-377.
- Deguchi T, Hatazaki K, Ito S, et al. Macrolide and fluoroquinolone resistance is uncommon in clinical strains of Chlamydia trachomatis. J Infect Chemother. Apr 4 2018.