Secondary switch to oral levofloxacin allowed early rehabilitation in primary ventriculitis caused by Neisseria meningitidis
A four-week antibiotic regimen combining two weeks of intravenous cefotaxime followed by two weeks of oral levofloxacin was shown to be effective in the treatment of meningococcal ventriculitis in an elderly.
An 85-year old man was admitted to the emergency department after a fall in the context of a fever at home but was afebrile at his arrival in the hospital. He had a history of atrial fibrillation requiring long-term curative anticoagulant therapy, kidney stones, and benign prostatic hyperplasia. Antibiotic was not prescribed as there was no evident diagnosis.
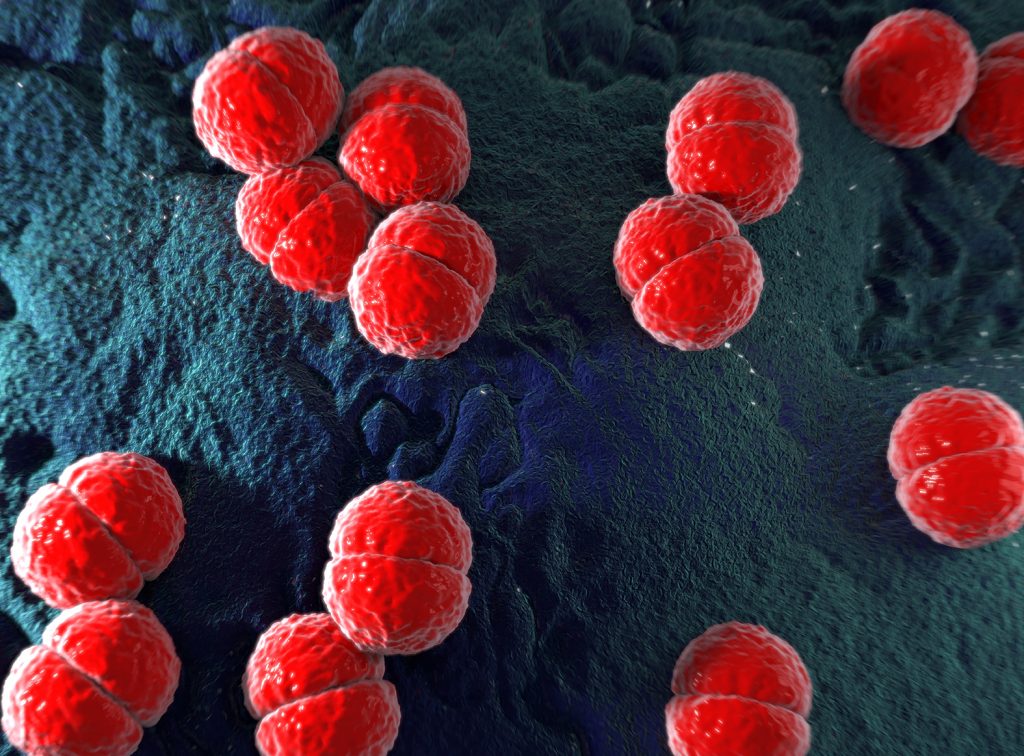
Two days later the patient’s condition worsened with high fever, confusion and altered mental status, with neither neck stiffness nor other symptoms of meningism. Diagnostic lumbar puncture revealed a purulent cerebrospinal fluid (CSF) with rare cocci of undetermined Gram staining observed on direct microscopic examination. Empiric therapy with intravenous (IV) cefotaxime and oxacillin in combination with adjunctive dexamethasone was initiated. A comatose state (Glasgow coma score 9/15) prompted his admission to the intensive care unit, intubation, and mechanical ventilation. A subsequent 24-hour CSF culture yielded a group B Neisseria meningitidis with reduced susceptibility to penicillin thus the removal of oxacillin from the patient’s antibiotic therapy.
The patient’s neurological state progressively improved and was extubated on day 5 of the combination treatment of cefotaxime and dexamethasone. He was discharged to the infectious diseases unit; however, he remained confused and somnolent (Glasgow coma score 14/15). Irregular intraventricular debris was observed in the lateral ventricles – a feature specific for pus which rules out acute blood clot, and which is reported in 94% if healthcare-associated ventriculitis.1 These unfavourable outcomes prompted a prolonged antibiotic therapy i.e., cefotaxime for 2 weeks followed by oral levofloxacin for another 2 weeks. Upon completion of the antibiotic treatment, the patient regained normal vigilant status and magnetic resonance imaging (MRI) showed reduction of purulent debris.
Only six cases of primary ventriculitis were reported in adults over the last decade, of which one was caused by N. meningitidis; however, five out of the previously reported cases and the current case had an atypical clinical presentation lacking meningism, a diagnostic feature of meningitis.2,3 In cases lacking clinical or biological specific parameters, MRI including gadolinium-enhanced sequences has allowed easier diagnosis of pyogenic ventriculitis and cerebral ventriculitis; MRI is also considered for patients who do not improve despite appropriate antibiotics, and to rule out embolic stroke, which present with blood clot.3
With the goal of reducing the intravenous (IV) treatment duration, the clinicians suggested an oral switch to levofloxacin to allow faster rehabilitation. Furthermore, levofloxacin has been shown to achieve good concentrations into the CSF.4,5 The relatively short 4-week treatment was validated by the absence of relapse.
In conclusion, this case demonstrates that levofloxacin is an easy-to-tolerate antibiotic that may be used for the treatment of pyogenic ventriculitis with atypical presentation.
Source
Primary bacterial ventriculitis in adults, an emergent diagnosis challenge: report of a meningococcal case and review of the literature.
PMID: 29776398
DOI: 10.1186/s12879-018-3119-4
Link: https://www.ncbi.nlm.nih.gov/pubmed/29776398
References
- Fukui MB, et al. AJNR Am J Neuroradiol 2001;22:1510-1516.
- Gronthoud F, et al. JMM Case Reports 2017;4: e005078.
- Lesourd A, et al. BMC Infect Dis 2018;18:226.
- Carbon C. J Chemother 2001;47:9-14.
- Chidiac C. Med Mal Infect 2015;45:348-373.










