Levofloxacin is associated with greater treatment success and lower mortality in pulmonary multidrug-resistant tuberculosis
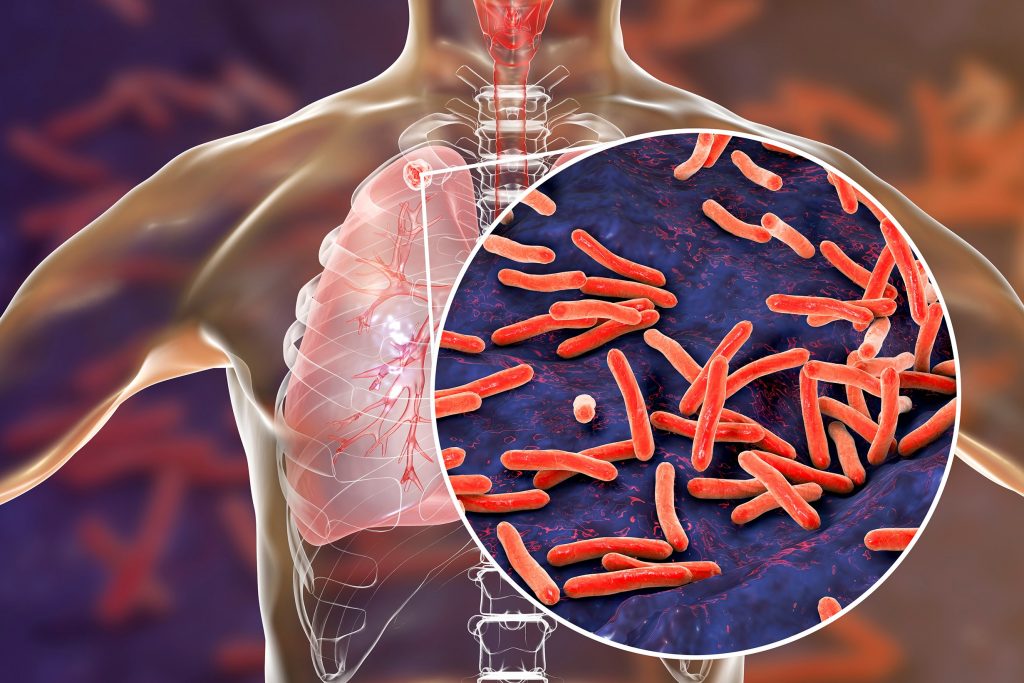
An individual patient data meta-analysis showed greater treatment success and lower mortality with the use of levofloxacin – compared with other second-line drugs – for pulmonary multidrug-resistant tuberculosis (MDR-TB).
The World Health Organization (WHO) had previously reported a relatively poor cure rate of 54% in patients with MDR-TB – attributable to longer treatment duration with second-line tuberculosis drugs which are less effective and more toxic than those used for drug-susceptible TB.1 There has been limited number of phase III clinical trials investigating the treatment regimen of MDR-TB. Therefore, this meta-analysis aimed to estimate the association of treatment outcomes with the use of existing anti-TB drugs.2
Treatment success was defined as being cured or having completed the course of treatment.2 Only the last completed treatment course (for at least one month) was taken into consideration for patients who received multiple courses of treatment; patients who received two or more drugs were excluded from the meta-analysis as treatment outcomes could not be attributed to any one of the drugs.2
The investigators reported better treatment outcomes if the isolate of Mycobacterium tuberculosis was susceptible to the drug used. Among patients, 61% (n=12,030) had treatment success – associated with the use of linezolid, levofloxacin, carbapenems, moxifloxacin, bedaquiline, and clofazimine; 8% had failure or relapse; and 14% died.2 Reduced mortality was also associated with the use of linezolid, levofloxacin, moxifloxacin, and bedaquiline. Compared with patients who did not receive any fluoroquinolones, patients whose isolates were resistant to ofloxacin, or patients with extensive drug resistance, treatment with levofloxacin or moxifloxacin was associated with significantly greater treatment success and lower mortality.2
The carbapenems and clofazimine were associated with greater treatment success in patients with MDR-TB, but not extensive drug resistance. Besides, among the second-line injectable drugs, amikacin was reported to have modest benefits while kanamycin or capreomycin had worse outcomes.2
This meta-analysis emphasises the importance of drug susceptibility testing to guide antibiotic selection, and the urgent need for clinical trials to assess the effectiveness and optimal treatment duration of individual drugs that were associated with treatment success.
Source
Treatment correlates of successful outcomes in pulmonary multidrug-resistant tuberculosis: an individual patient data meta-analysis.
PMID: 30215381
DOI: 10.1016/S0140-6736(18)31644-1
Link: https://www.ncbi.nlm.nih.gov/pubmed/30215381
References
- World Health Organization. Global tuberculosis report 2017. Available at: http://apps.who.int/medicinedocs/en/d/Js23360en/. Accessed October 2018.
- The Collaborative Group for the Meta-Analysis of Individual Patient Data in MDR-TB treatment–2017, et al. Lancet 2018;392:821-834.










