Ceftriaxone plus levofloxacin for the treatment of Streptococcus intermedius pleuropulmonary infection
Ceftriaxone–levofloxacin combination is the most frequently used antimicrobial for the treatment of Streptococcus intermedius pleuropulmonary infection; drainage of pleural effusion and other surgical procedures such as pleurectomy, thoracotomy, decortication, and debridement are recommended along with antibiotic therapy for treatment.
The S. anginosus group (SAG) – also known as the S. milleri group – includes S. intermedius, S. constellatus, and S. anginosus that are normal flora of the oral cavity, gastrointestinal and urogenital tracts but play important roles in respiratory infections.1 This group of streptococci has a propensity for abscess and empyema formation – a unique characteristic that distinguishes this group from other pathogenic streptococci.2 S. intermedius, in particular, has been associated with abscesses of the brain and liver.3 Over the past three decades, only a few cases of pleuropulmonary infection due to S. intermedius have been reported in medical literature.4-9
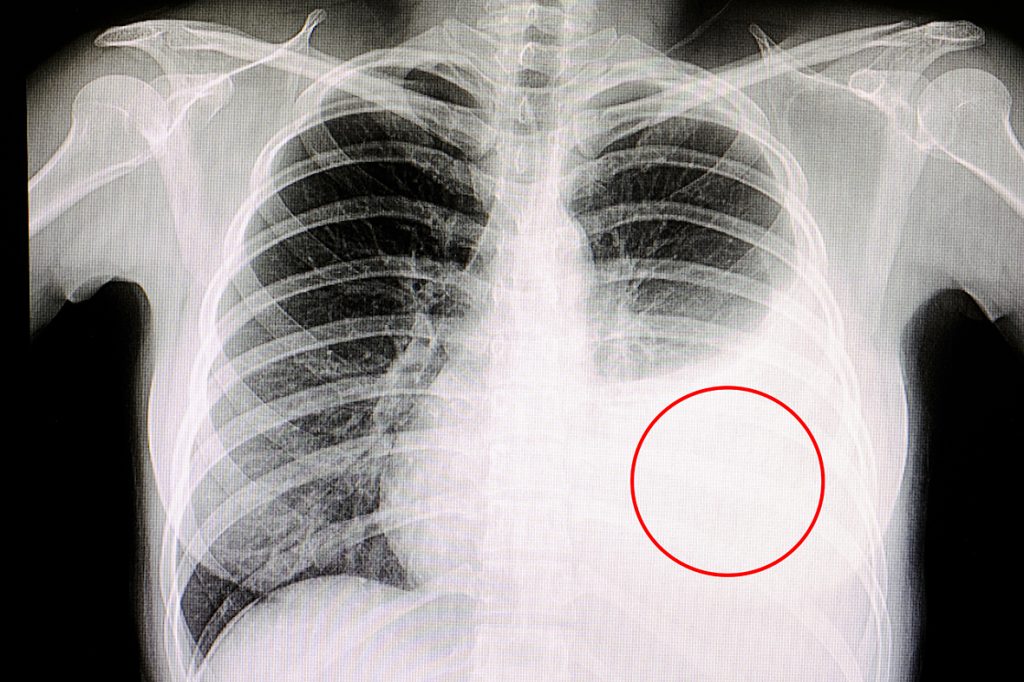
The authors of the present report describe the clinical and microbiological features of pleuropulmonary infection caused by S. intermedius based on six cases in the literature and nine cases presented at the Hospital Virgen de las Nieves in Spain.10 Predisposing risk factors for S. intermedius infection include alcoholism, periodontal disease, chronic obstructive pulmonary disease, diabetes mellitus, and tobacco use. Patients were often presented with two or more symptoms such as cough, chest pain, dyspnea, fever, empyema, pneumonia, and pleural effusion.
The mean diagnosis interval from the onset of symptoms was 34 days – S. intermedius was identified mainly from culture of pleural fluid aspirate and culture of biopsy or tissue samples.10 The microorganism is a Gram-positive, catalase-negative coccus that is nonmotile and is a facultative anaerobe.9 Elevation of white blood cell count (WBC) and C-reactive protein (CRP) level may suggest the presence of infection, but it is recommended that diagnosis be confirmed microbiologically as CRP is limited by poor specificity.10
Antimicrobial susceptibility was performed in nine of the cases – all isolates of S. intermedius were susceptible to cefotaxime, levofloxacin, linezolid, vancomycin, and daptomycin; 45.5% of isolates were resistant to both clindamycin and erythromycin; and one isolate showed intermediate susceptibility to penicillin.10 Ceftriaxone plus levofloxacin was the most commonly used antimicrobial regimen; antibiotic treatment along with drainage of pleural effusion and surgical treatment had favourable treatment outcomes.10
Pleuropulmonary infections are not commonly caused by S. intermedius.10 The authors recommend treatment of these infections to be guided by susceptibility studies although the combination of ceftriaxone–levofloxacin seemed to be the preferred antimicrobial therapy.
Source
Clinical and microbiologic characteristics of pleuro-pulmonary infection due to Streptococcus intermedius.
PMID: 29565100
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6159373/
References
- Noguchi S, et al. BMC Pulm Med 2015;15:133.
- Sunwoo BY and Miller Jr WT. Chest 2014;146:e121-e125.
- Whiley RA, et al. J Clin Microbiol 1992;30:243-244.
- Roy WJ, et al. J Ky Med Assoc 1991;89:558-562.
- Khatib R, et al. Clin Infect Dis 2000;30:396-397.
- Mautner GH, et al. Cutis 2000;65:318-320.
- Iskandar SB, et al. Tennessee Med 2006;99:37-39.
- Noguchi S, et al. Intern Med 2014;53:47-50.
- Hannoodi F, et al. Case Rep Pulmonol 2016;2016:7452161.
- Cobo F, et al. Rev Esp Quimioter 2018;31:146-151.










