Oral sitafloxacin as a switch therapy for the treatment of non-bacteraemic acute pyelonephritis
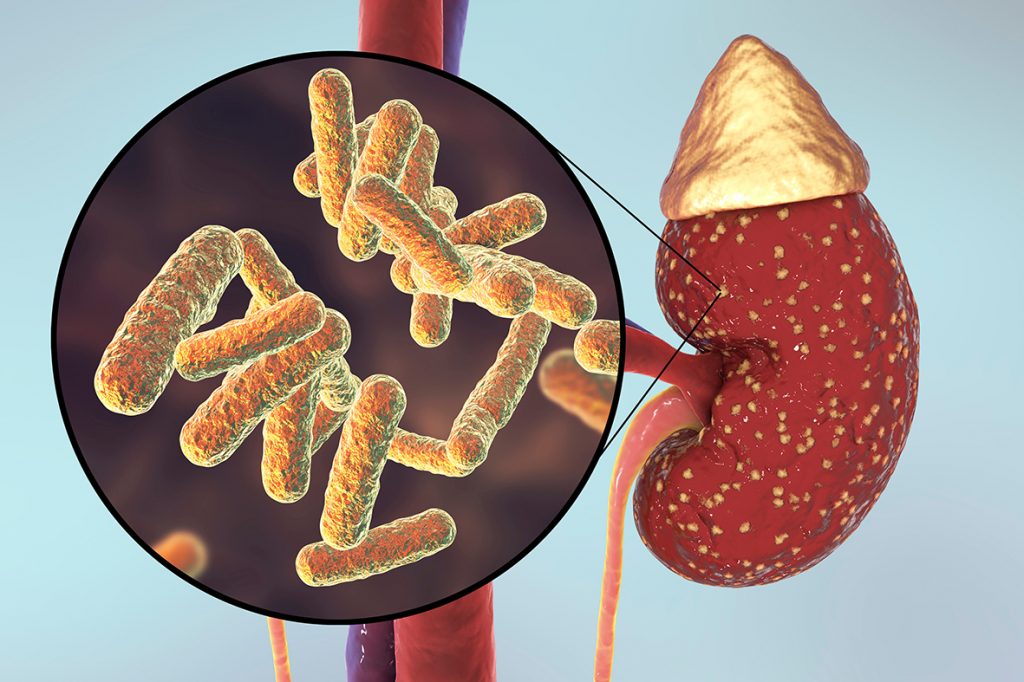
A treatment regimen of carbapenem followed by sitafloxacin or ertapenem was found to be effective in patients with non-bacteraemic acute pyelonephritis caused by extended-spectrum β-lactamase-producing Escherichia coli (ESBL-EC).
The incidence of urinary tract infections (UTIs) caused by ESBL-producing pathogens has been on the rise for the last few decades – particularly in outpatient settings, with ESBL-EC being a frequent cause of infection in the community and healthcare centres.1 However, treatment of ESBL-EC infection has been challenging due to their resistance to multiple antibiotics – limiting antibiotics choice to β-lactams/β-lactamase inhibitors, third- and fourth-generation cephalosporins, aminoglycosides, and fluoroquinolones.1 More recently, although carbapenems are frequently prescribed as empiric or definitive therapy, their widespread use has been associated with acquired and inherited antibiotic resistance.2,3
A prospective randomised controlled trial was conducted at Ramathibodi Hospital in Thailand from November 2012 to June 2015 to compare the effectiveness of sitafloxacin and ertapenem as a switch therapy for the treatment of non-bacteraemic acute pyelonephritis caused by ESBL-EC.1 The study aimed to identify an antibiotic substitute that could replace carbapenem for the treatment of this condition. Patients with presumptive diagnosis of acute pyelonephritis were randomised to receive oral sitafloxacin or intravenous (IV) ertapenem for 7 days; all patients received one of the IV carbapenems (meropenem 1 gm every 8 h, imipenem 500 mg every 6 h, doripenem 500 mg every 8 h, or ertapenem 1 gm once daily) for 3 days prior to randomisation.1
The clinical cure rate and bacterial eradication in the sitafloxacin group and ertapenem group were not significantly different i.e., 100% vs 94.1% (p=0.472) and 84.2% vs 75.0% (p=0.472), respectively.1 These findings indicate that the clinical efficacy of switch therapy from carbapenems to sitafloxacin was comparable to ertapenem in the management of non-bacteraemic acute pyelonephritis. The high clinical cure rate was attributable to the early detection of the disease – a median duration of 1 or 2 days.1 The safety profile and local tolerability of sitafloxacin were also similar to those of ertapenem.
In addition to its activity against multidrug-resistant (MDR) Gram-negative bacteria including ESBL-EC, the oral formulation of sitafloxacin eases the treatment of infections in both outpatient settings and hospitalised patients who do not require parenteral antibiotics.1 Previous studies have also demonstrated equivalent effectiveness of fluoroquinolones and carbapenems in patients with ESBL-EC and ESBL-Klebsiella pneumoniae (ESBL-KP) bacteraemia.4,5 Ertapenem is also an ideal antibiotic of choice for the treatment of UTIs, particularly for patients in nursing homes and outpatient settings because of its once-daily dosage.6,7
Considering its favourable clinical and microbiological outcomes, the authors concluded that sitafloxacin may be considered as an alternative antibiotic choice of switch therapy in acute pyelonephritis caused by ESBL-EC.
Source
A randomized controlled trial of sitafloxacin vs. ertapenem as a switch therapy after treatment for acute pyelonephritis caused by extended-spectrum β-lactamase-producing Escherichia coli: A pilot study.
PMID: 28587974
DOI: 10.1016/j.jiac.2017.05.005
Link: https://www.ncbi.nlm.nih.gov/pubmed/28587974
References
- Malaisri C, et al. J Infect Chemother 2017;23:556-562.
- Bradford PA. Clin Microbiol Rev 2001;14:933-951.
- Cunha BA. Semin Respir Infect 2002;17:231-239.
- Kang CI, et al. Antimicrob Agents Chemother 2004;48:4574-4581.
- Nakashima M, et al. Antimicrob Agents Chemother 1995;39:170-174.
- Alhambra A, et al. J Antimicrob Chemother 2004;53:1090-1094.
- Mody RM, et al. Ann Clin Microbiol Antimicrob 2007;6:6.










