CDC updates treatment guidelines for gonococcal infection
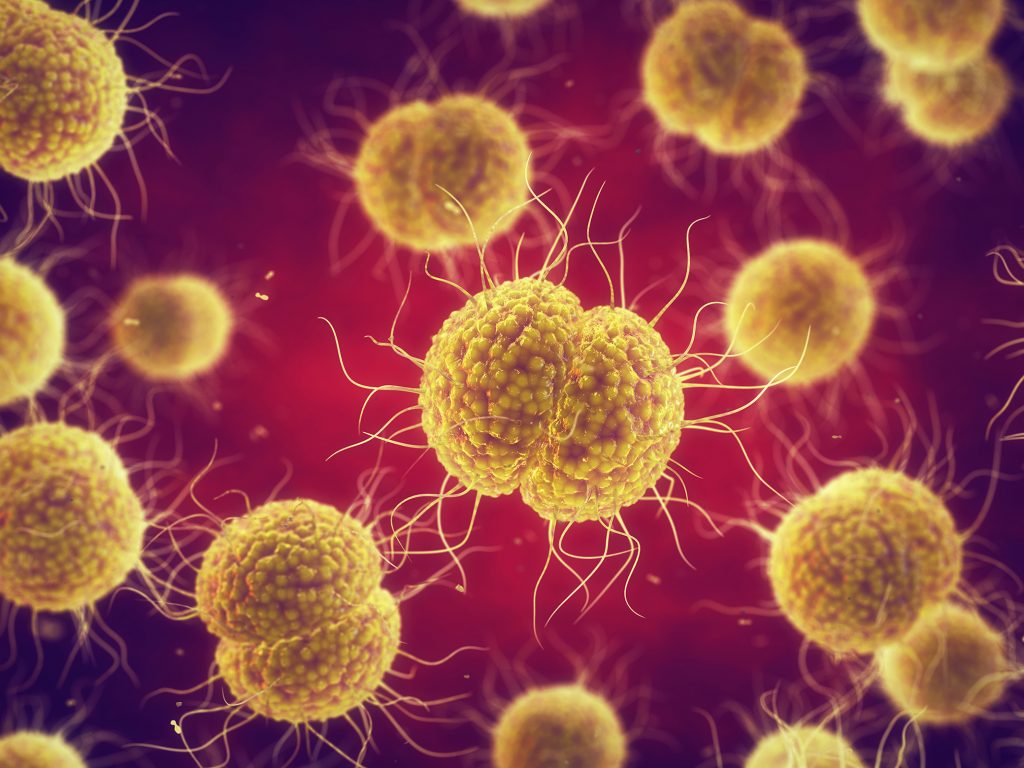
Gonorrhoea – caused by infection with the Neisseria gonorrhoeae bacterium – affects approximately 106.1 million people annually, with rates of infection increasing steadily over the last few years.1-4 While the disease is a non-complicated mucosal infection in most cases, untreated gonorrhoea can cause serious and permanent health issues, with complications including sterility, ectopic pregnancy, septic arthritis, and sometimes death.3,5 Worldwide, N. gonorrhoeae strains now show increasing resistance to most antimicrobials that are widely used to treat the disease, raising concerns about the eventual development of untreatable gonococcal infections and the need to re-evaluate the current usage of antimicrobials.4-6
Given the major public health threat of this evolving ‘superbug’, the Centers for Disease Control and Prevention (CDC) has updated its gonococcal treatment guidelines to address the appropriate use of antimicrobials and the potential impact of dual therapy on commensal organisms and concurrent pathogens.7
Highlights of the revised treatment guidelines include7:
- For treatment of uncomplicated urogenital, rectal, or pharyngeal gonorrhoea, a single 500 mg intramuscular (IM) dose of ceftriaxone should be administered, instead of the 2010 recommendation of a single 250 mg IM dose of ceftriaxone + single 1 g oral dose of azithromycin.
- The pharmacokinetic and pharmacodynamic properties of ceftriaxone mean that a 500 mg dose in an average-weight U.S. adult achieves sufficiently high serum levels for an adequate duration to eradicate infection, even with wide pharmacokinetic variability.
- The high frequency of pharyngeal gonorrhoea with substantial underscreening and the increased understanding of wide individual pharmacokinetic and pharmacodynamic variability has contributed to the recommendation for the increased ceftriaxone dose.
- If chlamydial infection has not been excluded, providers should treat for chlamydia with oral doxycycline (100 mg twice a day for 7 days).
Pivoting from combinational therapy with azithromycin to ceftriaxone monotherapy is an important step in curtailing antibiotic resistance, as N. gonorrhoeae remains highly susceptible to ceftriaxone and the rate of azithromycin resistance continues to increase.7 The prudent use of antimicrobial agents and monitoring for emergence of ceftriaxone resistance through surveillance and health care providers’ reporting of treatment failures will be essential to ensure efficacy of recommended regimens.7
References
- Piszczek J, et al. Can Pharm J (Ott) 2015;148:82-89.
- World Health Organization. Sexual and reproductive health. Available at: https://www.who.int/reproductivehealth/publications/rtis/stisestimates/en/. Accessed 29 Jan 2021.
- Hill SA, et al. Microb Cell 2016;3:371-389.
- Bodie M, et al. Can Commun Dis Rep 2019;45:54-62.
- Pan American Health Organization. Gonorrhea. Available at: https://www.paho.org/hq/index.php?option=com_content&view=article&id=14872:sti-gonorrhea&Itemid=3670&lang=en#:~:text=The%20estimated%2027%20million%20prevalent,of%20people%20with%20gonorrhea%20worldwide. Accessed 29 Jan 2021.
- Unemo M, Shafer WM. Clin Microbiol Rev 2014;27:587-613.
- Centers for Disease Control and Prevention. Update to CDC’s Treatment Guidelines for Gonococcal Infection, 2020. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/mm6950a6.htm?s_cid=mm6950a6_w. Accessed 29 Jan 2021.