Bacterial coinfection found to be prevalent among hospitalised patients with community acquired pneumonia and flu
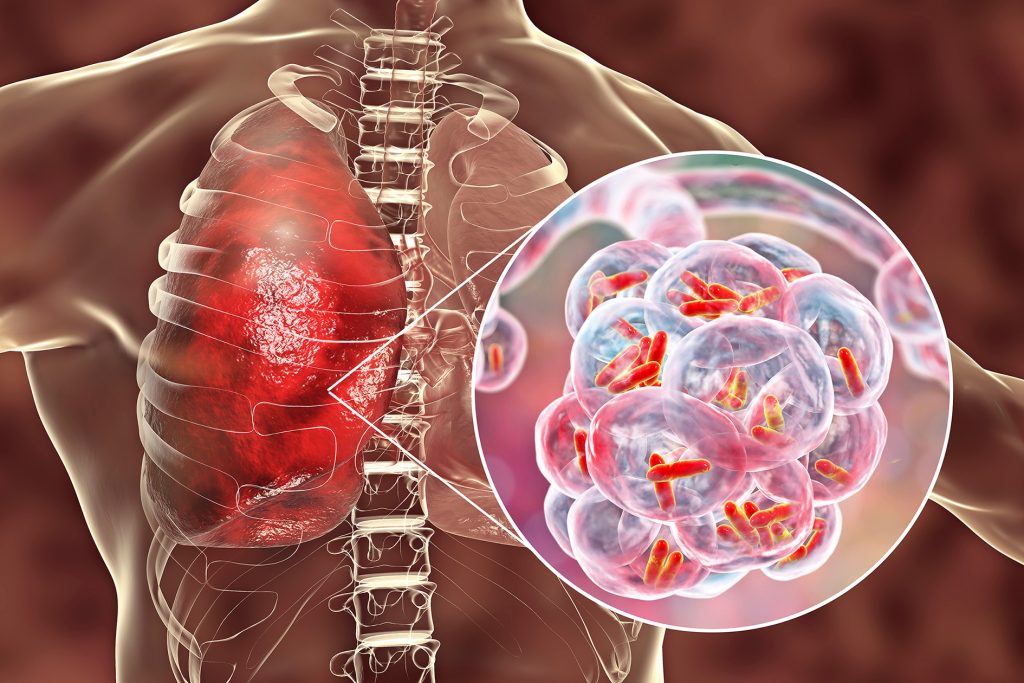
Influenza (or flu) is a contagious viral infection of the respiratory tract.1 It is estimated that over five million hospitalisations per annum worldwide are associated with influenza viruses, with the highest risk among those older than 65.2 One third of pneumonia cases are caused by viral infections, including the flu,3 and interactions between influenza and pneumonia-causing bacteria have been reported in pandemic, epidemic, and seasonal influenza.4
The Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS) currently recommend that patients hospitalized with community acquired pneumonia (CAP) who test positive for influenza should receive antibiotics targeting typical CAP pathogens as bacterial coinfection is frequent.4 They do, however, recognise that patients with influenza could stand at an increased risk for coinfection with Staphylococcus aureus or other bacteria associated with the flu.4
Hoping to better inform treatment decisions, Bartley et al. collated data of adult inpatients admitted with CAP who were also tested for concomitant influenza infection across 179 hospitals in the United States from 2010 to 2015 (non-pandemic years). 4 Their analysis aimed to elucidate trends in bacterial coinfection, corresponding bacterial distribution and their relation to in-hospital mortality, disease deterioration, and costs.
Of 38,665 patients hospitalized with CAP, 11.2% tested positive for influenza.4 Based on the results of blood and respiratory cultures within the first 3 days of hospitalization, an estimated 10.3% of patients with influenza had community-onset bacterial coinfection, compared with 16.2% of patients without influenza (p<.001).4 Staphylococcus aureus was also more common among patients with influenza (34.2% vs 28.2%, p=.007), and Streptococcus pneumoniae less so (24.9% vs 31.0%, p=.008).4 It was notable, however, that S. aureus isolates from influenza patients were less likely to be methicillin resistant (42.8% vs 53.2%, p=.01).4
Other key findings from Bartley et al.’s study include4:
- Differences in rates of aureus and S. pneumoniae bacterial coinfection were only present in the first 3 days, which reflects the effect of nosocomial pathogens as hospital stay prolongs.
- Bacterial coinfection was associated with higher risk of inpatient costs, worse disease progression (including late transfer to ICU, late use of mechanical ventilator or vasopressors, etc.) and increased mortality.
The IDSA’s previous treatment guidelines for influenza pneumonia (published alongside the Centers for Disease Control and Prevention) suggests the use of broad-spectrum antibiotics for patients presenting with severe disease.5 However, the results from this study which observed a lower incidence of methicillin resistant S. aureus (MRSA) in influenza pneumonia cases within the first 3 days of hospitalisation support the recent guideline update by IDSA/ATS for CAP, where MRSA coverage should no longer be routinely provided, and should be reserved for patients with known risk factors for MRSA instead.
References
- Center for Disease Control and Prevention. Key Facts About Influenza (Flu). Available at: https://www.cdc.gov/flu/about/keyfacts.htm. Accessed 7 June 2021.
- Lafond KE, et al. PLOS Medicine 2021;18:e1003550.
- John Hopkins Medicine. Pneumonia. Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/pneumonia. Accessed 7 June 2021.
- Bartley PS, et al. Infect Control Hosp Epidemiol 2021;doi:10.1017/ice.2021.96. [Epub ahead of print]
- Uyeki TM, et al. Clin Infect Dis 2019;68:895–902









