Helicobacter pylori infections: A review of the current standard of care
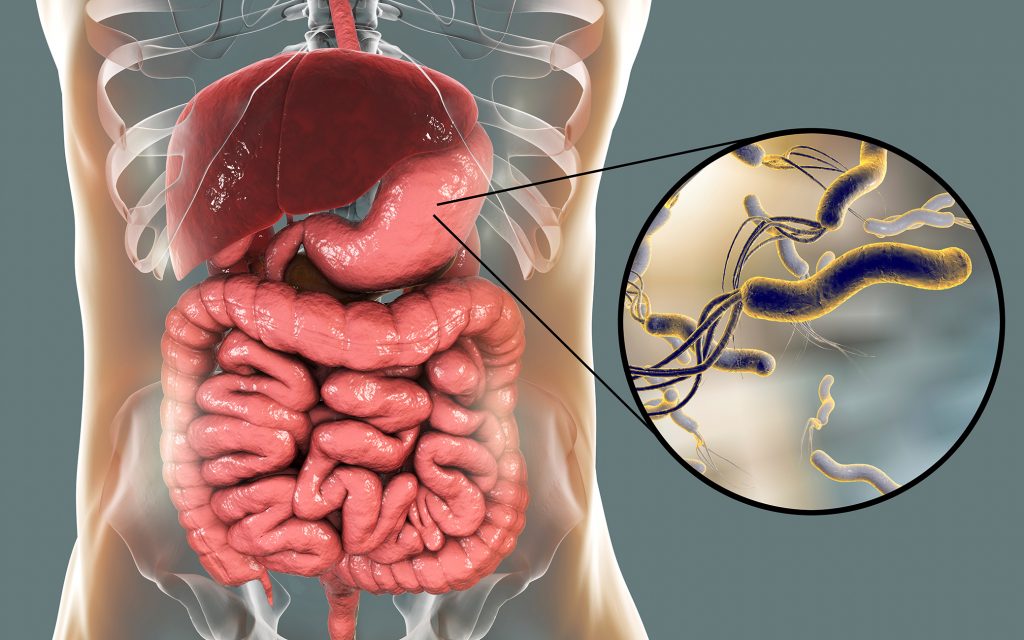
In 2015, approximately 4.4 billion Helicobacter pylori infections were reported worldwide.1 Prevalence of H. pylori infections varies across countries, with more industrialised countries showing a plateau or decline in infection rates, but even in Switzerland, the country with the lowest infection rates, prevalence stands at 18.9%.1 Efforts to eradicate this disease and its associated sequelae (chronic gastritis, peptic ulcers, gastric cancer) are ongoing, but there is a lack of standardised treatments across the globe, with some treatments potentially risking gut flora dysbiosis.2-4 Furthermore, indiscriminate use of antibiotics for medical and veterinary purposes has also led to increased antimicrobial resistance in this gram-negative bacterium.3 As such, there is a pressing need for standardised treatment guidelines for H. pylori infections to minimise the associated risks.
Researchers from Nihon and Kitasato universities, Japan, reviewed current international treatment guidelines (including guidelines from the American College of Gastroenterology, and consensus reports from several countries and cities, namely Japan, Korea, China, Toronto, and Maastricht) and a network meta-analysis of H. pylori treatment outcomes to determine the current optimal treatment for H. pylori infection.3 H. pylori infection induces an ongoing state of inflammation that increases the risk of its associated sequalae.3 As such, current treatments typically aim to reduce inflammation while clearing the infection, and often include a proton pump inhibitor (PPI) and a combination of antibiotics.
Current international guidelines recommend the following H. pylori treatments3:
- Nonbismuth quadruple therapies (including concomitant quadruple and reverse hybrid therapies) for 10–14 days.
- Concomitant quadruple therapy: esomeprazole (20 mg), amoxicillin (1000 mg), clarithromycin (500 mg), and metronidazole (500 mg) twice daily.
- Reverse hybrid therapy: dexlansoprazole (60 mg) once daily; clarithromycin (500 mg), metronidazole (500 mg) twice daily for the first 7 days; amoxicillin (1000 mg) twice daily for the full 14-day treatment period.
- Vonoprazan-based triple therapy (20 mg vonoprazan, 750 mg amoxicillin and 200 mg clarithromycin twice daily) for 7 days.
While these treatment regimens have exhibited successful eradication rates (~90%), even in regions with high prevalence of resistant strains, concurrent use of multiple antimicrobials still poses the risks of increased antimicrobial resistance and disturbance of natural gut microflora.3 The emergence of resistant H. pylori strains reduces treatment efficacy, therefore an ideal treatment regimen should aim to maintain eradication efficacy while reducing antibiotic consumption.3
As such, a shift to alternative regimens is required, which include3:
- High-dose dual therapy combining a PPI (minimum twice daily) with amoxicillin (> 2000 mg daily).
- This treatment is often used as a rescue for ineffective or failed pylori treatments.
- However, relatively lower patient compliance due to high dose, increased frequency and long duration of treatment pose limitations to this regimen.
- Dual therapy with vonoprazan (20 mg) and amoxicillin (750 mg) twice daily for 7 days.
- Several studies have shown efficient eradication rates (85–93%) for this treatment, comparable to current standard of vonoprazan triple therapy.
- This treatment was shown to exert less of a negative impact on gut microbiota compared to vonoprazan triple therapy.
- Maintaining bactericidal concentrations of amoxicillin by increasing treatment dose or administration frequency could be considered to improve efficacy.
The vonoprazan-amoxicillin dual therapy is a simple treatment regimen with minimal disruption to natural gut microflora.3 The regimen provides favourable eradication rates and improves safety and tolerability, including reducing the risk of emergent antimicrobial resistance.3 These important findings could inform future international guidelines for the treatment of H. pylori infection in the ongoing battle against antimicrobial resistance.
References
- Hooi JKY, et al. Gastroenterology 2017;153:420-9
- Guevara B, Cogdill AG. Dig Dis Sci 2020;65:1971-1931
- Suzuki S, et al. Digestion 2022;103:62-68
- Kuipers EJ, et al. The Lancet 1995;345:1525-1528










