60-year development of quinolones: The clinical application of quinolones in urology
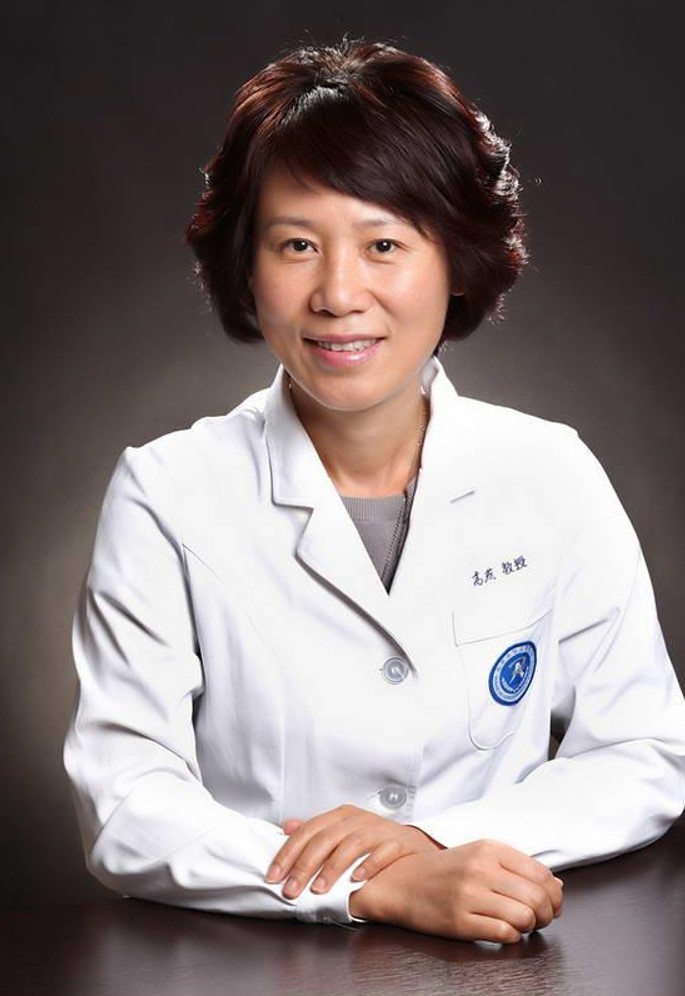
Gao Yan, Chief Physician, Professor, Doctoral Supervisor
- Member of the Medical Treatment Expert Group for Covid-19, National Health Commission
- Director of the Department of Infectious Diseases, Director of the Department of Infection Control, Peking University People’s Hospital
- Specialties: Diagnosis and treatment of febrile diseases, complicated infections, and infection prevention and control
- Winner of the 4th “National Famous Doctor – Outstanding Achievement” awarded by Chinese Medical Association
- Member of Infectious Diseases Branch, Chinese Medical Association
- Committee member of the Infectious Diseases Committee, Chinese Medical Doctor Association
- Committee Member of the Special Committee on Rational Use of Antibacterial Drugs, Chinese Hospital Association
- Committee Member of Infection Control Branch, Chinese Preventive Medicine Association
- Vice Chairperson of the Infectious Diseases Special Committee, Beijing Medical Doctor Association
- In charge of the sub-project of the National Science and Technology Major Project “Technology Research on Rapid Detection Platform of Respiratory Infectious Pathogens”, the National Natural Surface Project “The Law of Cooperative Mutation of Surface Antigen of New Influenza A H1N1 Virus and Its Influence Mechanism on the Biological Characteristics of the Virus”, and several national and provincial-level projects such as “Research on the Monitoring Platform for Adult Community-Acquired Pneumonia in Beijing Area” conducted by the Beijing Association for Science and Technology.
- Published more than 110 journal articles in SCI and core journals as the first or corresponding author. Engaged in the compilation and translation of more than 20 medical textbooks and monographs. Participated in the compilation of domestic industry guidelines and expert consensus.
Quinolones have been developed into a fourth generation, and for the past 60 years they have provided numerous clinicians with extensive clinical experiences, which has enabled us to gain better insights into the clinical application of quinolones in urology. Ciprofloxacin and levofloxacin are widely used in treating urinary tract infections owing to advantages such as good oral bioavailability, high urine concentration, and once daily administration.1,2 The launch of the novel quinolone ‘sitafloxacin’ serves as a new treatment option for treating urinary tract infections.
- The value and status of traditional classic quinolones in the treatment of urinary tract infections (UTIs)
UTIs are usually classified as upper or lower according to where they occur along the urinary tract; they may be further divided into complicated and uncomplicated UTIs, and the difference is whether complicated factors are involved.3 Additionally, there are some special types of UTIs, such as urinary tract infection before and after stone surgery, catheter-related urinary tract infection, etc. Some complicated urinary tract infections may lead to uremia, which is a clinical emergency.3
In addition to the types of infection, the bacterial strain of the infection should also be the focus of the anti-infective treatment of urinary tract infection. The top five pathogenic bacteria of urinary tract infection are Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, Enterobacter cloacae and Staphylococcus aureus.4 In immunocompromised patients, nonfermenters such as Pseudomonas aeruginosa and Acinetobacter baumannii may be detected. Currently, in China, the drug resistance of extended-spectrum β-lactamase (ESBL)-producing Escherichia coli is a deteriorating problem which has posed a challenge to clinical treatment.5
In the anti-infective treatment of urinary tract infections, fosfomycin, nitrofurantoin, sulfonamides, and quinolones are recommended oral drugs.6 Among quinolones, levofloxacin in particular, the urine concentration is more than 100 times higher than the plasma concentration, so it is often found in clinical practice that ESBL-producing Escherichia coli are resistant to levofloxacin in urine culture reports; however, the clinical application proves to be effective. The chief reason is that MIC values are determined based on plasma concentration.7
The extensive application of quinolones in clinical practice derives from their features such as intravenous injection, oral sequential and once-daily administration, safety etc. For the past 60-plus years since quinolones were launched, countless patients have benefited from them.
- The need of anti-infective treatment options combined with local etiological distribution, drug resistance traits, and factors related to national conditions
Between the “Guidelines for the Diagnosis and Treatment of Urinary System Infections in China” and the “European Association of Urology (EAU) Guidelines for Urinary Infections,” certain differences exist with regard to the recommendation of quinolone antibiotics. The selection of anti-infective drugs varies mainly owing to differences in the distribution of pathogens, drug resistance, drug availability, patient acceptance, and medical insurance.8 In addition, the differences in national conditions among countries must be taken into consideration. In some countries, for example, fewer patients and sufficient hospital bed capacity enables patients with upper urinary tract infection to be admitted to hospital. In China, on the other hand, complicated urinary tract infections are generally treated in outpatient clinics due to the large number of patients and an undersupply of hospital beds. Owing to multiple disparities, quinolones can be administered both intravenously and orally once a day to meet the needs of clinicians and patients in China.
- New treatment options provided by the novel quinolone sitafloxacin for treating urinary tract infections
Sitafloxacin has strong antibacterial activity against Gram-negative bacteria, including the infection of nonfermenting Pseudomonas aeruginosa,9 for which efficacy is superior to levofloxacin. The indications for sitafloxacin include community-acquired pneumonia and urinary tract infection. The application in clinical practice indicates that sitafloxacin is equally effective and relatively safer compared to levofloxacin.9
Despite its enhanced antibacterial activity against Gram-negative bacteria, sitafloxacin can only be administered orally, and thus it is not the drug of choice for treating patients with severe infections or multidrug-resistant infections; however, for moderately or severely infected patients, sitafloxacin can be used for sequential treatment and discharge medications.10
References:
- Instructions on Ciprofloxacin
- Instructions on Levofloxacin
- EAU Guidelines on Urological Infections. 2021.
- Hyun-Sop Choe, et al. 2018; 24(4):278-283.
- Huang Xun, et al. Chinese Journal of Infection Control. 2015.14(1):1-9.
- Bonkat, et al.EAU Guidelines on urological infections. 2020.
- Xu Xirong, et al. Journal of Qiqihar Medical College. 2011.1:16-18.
- Chinese expert consensus on the diagnosis and treatment of urinary tract infection. Chinese Journal of Urology, 2015, 36(4):241-244.
- Instruction on Sitafloxacin in China.
- Chitprasong Malaisri, et al. J Infect Chemother. 2017; 23(8):556-562.










